What’s “Normal” In the Slow Fade of a Pandemic?
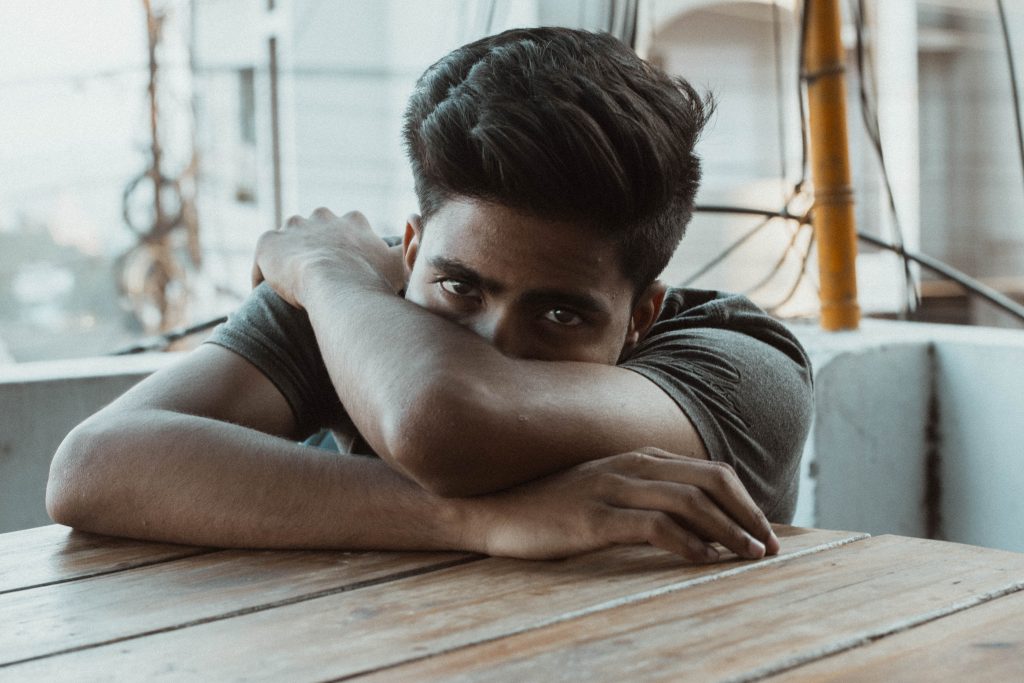
Even as the pandemic begins a slow fade, the mental health crisis that the pandemic ignited in kids, teens grownups, and caregivers for elders is sticking around. In my therapy office of late, I’ve heard clients name rumination, depression, grief, more alcohol and marijuana, new existential questions about meaning and purpose, relationship challenges, parenting stress, exhaustion, preoccupation about weight, intrusive thoughts, and lots and lots and lots of anxiety (social anxiety, health anxiety, traveling anxiety, etc.) In fact, we now have a name for all the inner debris that the pandemic has left in us: Post Pandemic Stress Disorder. This is on top of all the stress, anxiety, depression, and relationship stuff many of us carry around even in non-pandemic days.
So here are a few points I wish we could all keep track of:
1: Sometimes my clients think that if an event is over, they should be over it. But our brains, nervous systems, and bodies don’t work like light switches. Rather our nervous systems are like cars — needing time to rev up and time to slow down. So it’s normal to not feel normal right now. It’s normal to be experiencing residual exhaustion, more sensitivity to stressors, and to generally feel on edge and like you don’t quite have your social sea legs. Does this mean it’s fun? No. But is having a disrupted nervous system normal given the completely abnormal last 16 months? Yes. Absolutely, yes.
2: During the last year plus, we’ve all been taking stock of our lives: what we like, what we don’t like, what we want more of, and what we want less of in our lives. If you are still looking around trying to figure out what you want your new normal to include and exclude, you are doing something important – and normal. Many of us have had a break from friends, commutes, social obligations, work travel, etc. and now, to some extent, we have some choices in front of us. Do we want to socialize more, less, or differently than before the pandemic? Do we want to advocate for different hours or different amounts of times at our jobs? Do we want to set different boundaries with our families or around our time? These questions are normal. And it’s normal to re-evaluate our priorities following a big, terrible event.
3: If you have gained weight during the last 16 months, congrats on being normal. As far as coping strategies go, eating a bit more than we need is not the worst thing ever. We’ve been going through an ongoing trauma, and our bodies naturally crave sugar and salt when we’re stressed. I hope you can give yourself a break over the weight gain. And maybe even learn about the Health At Every Size movement. Or if you can’t be kind to yourself about your body, please come see me and and let me give you a break.
4: Finally, if you’re feeling bad for feeling bad (as in “I have so much privilege, I don’t deserve to be having a hard time”) then congrats – also normal. Think of this like survivor’s guilt. There’s a guilty feeling that’s hard to shake. But guess what – this too is normal. And while I know it’s hard to stop guilt once it’s ramped up, your guilt does not help anyone.
So – what to do? Consider self-compassion. Surround yourself with people who will be supportive and not make you feel like a weirdo (unless you’re a weirdo in all the good ways). Remind yourself that your experience can be normal AND still be really, really hard. And help your nervous system know it’s now safe to calm down: through regular sleep, nourishing food and relationships, movement, time outside, and – the hardest for many of us – not pushing yourself too hard. Does all that sound impossible? If so, no worries… that’s normal too (and why we therapists are here).